Type 1 Diabetes is explained as simply as possible…
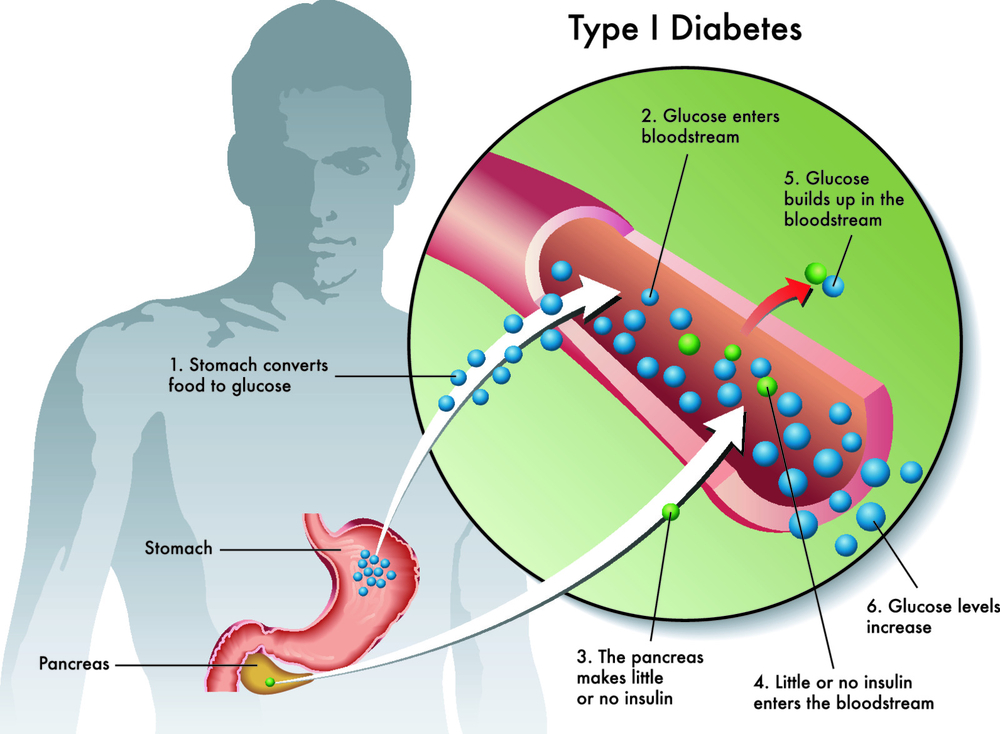
When you have diabetes, an increase in blood glucose levels occur when glucose can’t get into your fat and muscle cells where it is needed. For a cell in your body to gain glucose access, it needs a small molecule called insulin. This ‘key molecule’ unlocks the door into the cell. People with Type 1 Diabetes no longer produce insulin for any number of reasons.
Type 1 Diabetes explained in a little more detail…
THE NUMBER OF PEOPLE WITH TYPE 1 DIABETES IS INCREASING EACH YEAR.
Latent autoimmune diabetes in adults (LADA)
Latent from the Latin words Latere meaning hidden, or it comes on quite slowly as to appear it was hidden. LADA's signs and symptoms have a slower course of onset compared to Type 1 diagnosed in children, sometimes developing over a period of years. Latent autoimmune diabetes in adults, or LADA, is a form of Type 1 diabetes occurring in adulthood. Because these symptoms develop slowly, LADA can sometimes be incorrectly diagnosed as type 2 diabetes in adults.
Some of the characteristics of LADA include:
- Age of onset is 30 years and older
- Healthy weight with BMI is less than 25kg/m2
- Personal or family history of autoimmune disease
- Gradual onset

Who is at risk of Type 1 Diabetes?
It is more likely if someone in your family has Type 1 or perhaps another autoimmune disease like celiac disease, Addison's disease, pernicious anemia, or autoimmune thyroid disease. It can occur at any age but typically doesn’t develop in the first year of life. Even though it is often associated with children, half the people who develop Type 1 are over 30.
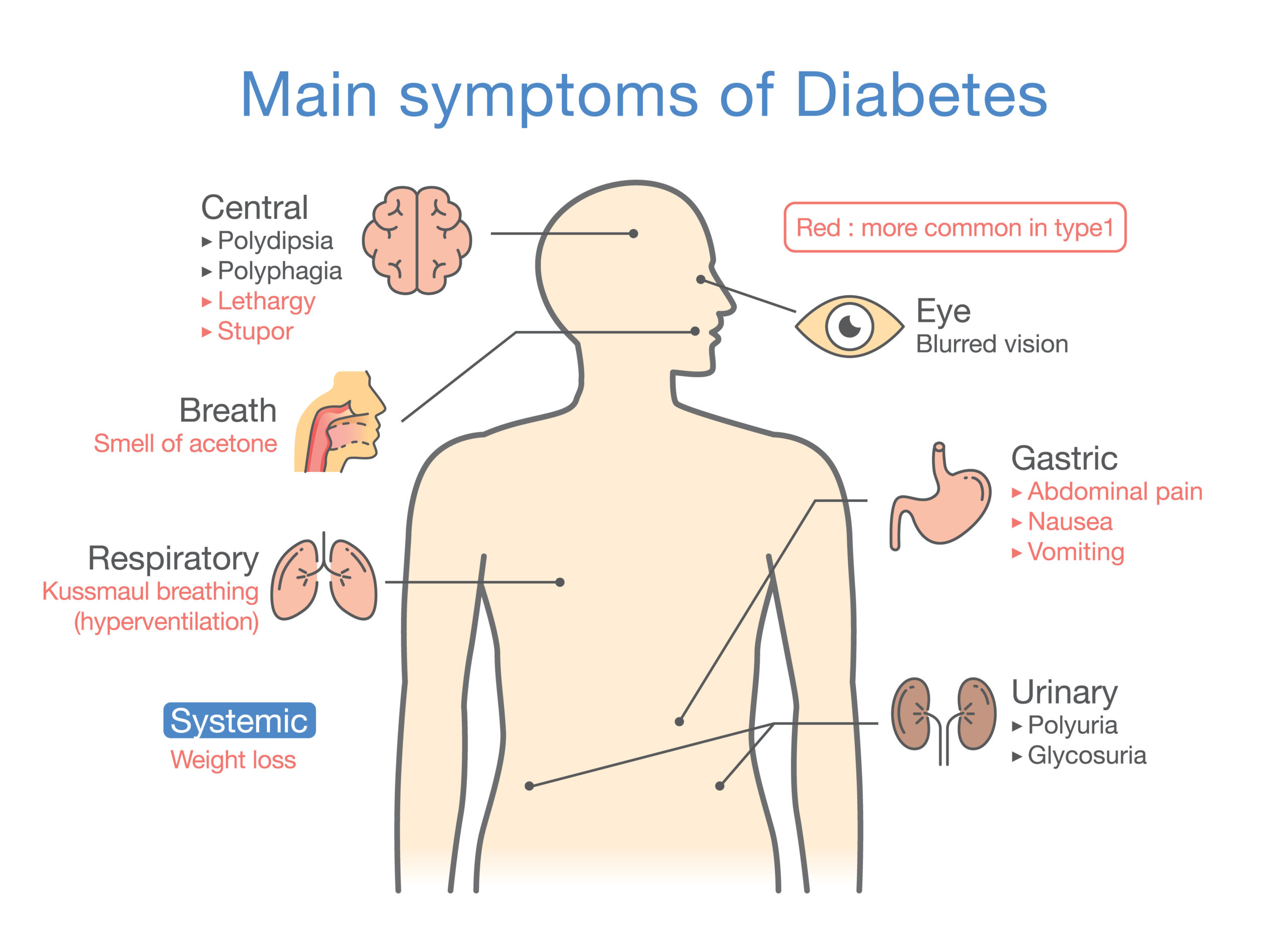
What are the symptoms of type 1 Diabetes?
Type 1 Diabetes and Diabetic Ketoacidosis
Diabetic ketoacidosis (DKA) is a condition that occurs due to a build-up of poisonous chemicals, called ketones, in the bloodstream. DKA occurs in approximately 30% of children who present with Type 1 Diabetes. This causes the blood to become acidic, and the combination of acids and dehydration can lead to comas and potentially death.
In a person who has Type 1 Diabetes, the body cannot use glucose for energy. Instead, stored fat in the body is used as a source of energy. The breakdown of these fatty acids results in the build-up of ketones, which can also appear in your urine.
Some symptoms of DKA include:
- Moderate to heavy ketones in the urine
- Rapid breathing
- Flushed cheeks
- Abdominal pain
- Sweet acetone (like nail polish remover) smell on the breath
- Vomiting
- Dehydration
Complications of untreated Type 1 Diabetes
Complications of Type 1 Diabetes are all related to poor blood glucose control. Poor control of blood glucose levels over several years can affect the blood vessels in the body, resulting in problems with the small blood vessels (known as microvascular complications) or the large blood vessels (known as macrovascular complications). The blood vessels' effects from ongoing uncontrolled blood glucose levels are a major source of morbidity and mortality for people with diabetes.
Microvascular complications – problems with small blood vessels
Like a macrovascular disease, ongoing high blood glucose levels are an important risk factor for developing a microvascular disease in patients with type 2 diabetes.
Microvascular complications include:
- Retinopathy – Disease of the eye which can lead to blindness
- Neuropathy – Disease of the nerves which can lead to foot ulcers requiring amputation
- Nephropathy – Disease of the kidneys which can lead to kidney failure and the need for dialysis
Diabetic retinopathy is the most common microvascular complication of diabetes. One in three people living with diabetes has some degree of diabetic retinopathy, and every person who has diabetes is at risk of developing it.
Macrovascular complications – problems with large blood vessels macrovascular disease affects the larger blood vessels in our body that supply blood to the heart, brain, and legs.
Macrovascular complications include:
- Coronary artery disease can lead to a heart attack
- A cerebrovascular disease which can lead to a stroke
- Peripheral artery disease can lead to pain deep in the leg muscles (calves, thigh, or buttocks) during activity and amputations.
Diabetes increases the risk that a person will develop cardiovascular disease than someone who does not have diabetes. In fact, cardiovascular disease is the primary cause of death in people with Type 1 Diabetes.
You are not alone. Learn how to regain control of your blood glucose, join our Diabetes Direct Care™ program. When you sign up, you’ll have 24/7 care 365 days a year—our telehealth (unlimited virtual visits, text, or email communications) -second to none.
Tests diagnosing Type 1 diabetes mellitus include:
This test requires a person to fast for over eight hours, followed by a blood test. A fasting plasma glucose greater than 7 mmol/L or 126 mg/dL on more than one occasion may indicate diabetes.
A random blood glucose test is taken at any point… it’s random! A reading of 11.0mmol/L or 200mg/dL or more can indicate classic symptoms of hyperglycemia (high blood glucose levels).
An oral glucose tolerance test (OGTT) involves consuming a sugary glucose syrup followed by a blood test one hour later and another two hours later. A plasma glucose reading of 11.0mmol/L or 200mg/dL or more at the two-hour blood test can indicate diabetes.
The Hb A1c test looks at the amount of glucose that is bound to a particular type of hemoglobin, the oxygen carrying molecule in your blood. A person's Hb A1c can be a good indication of average blood glucose control, as it shows the average blood glucose levels over a 2-3 month period. A reading of 6.5% or more can indicate diabetes. However, measured Hb A1c may not be truly reflective of blood glucose control in some people.
A PERSON WITH TYPE 1 DIABETES WILL DO AROUND 120,000 BLOOD TESTS OVER A LIFETIME.
How is type 1 Diabetes treated?
In Type 1 Diabetes, treatment involves two key factors:
- Checking blood glucose levels regularly to make sure they aren’t too low or too high, and
- Using insulin (through a pen or pump) to help keep blood glucose levels in a safe range
Insulin is the main treatment for people with Type 1 Diabetes. The goal of insulin therapy is to replace the insulin no longer being produced by the pancreas to achieve normal glucose. Since insulin is a crucial hormone that allows glucose in the bloodstream to get into the muscle and fat cells, replacing insulin is necessary for people with Type 1 Diabetes. There are many different types of insulin and can be classified by the onset and duration of action.
These include:
- rapid-acting insulin
- intermediate-acting insulin
- long-acting insulin
Intensive insulin therapy can be delivered by either multiple daily injections (MDI) or through continuous insulin infusion (pump).
In the Diabetes Control and Complications Trial (DCCT), it was found intensive therapy aimed at lower levels of blood glucose resulted in decreased rates of retinopathy, neuropathy, and nephropathy in people with Type 1 Diabetes (The Effect of Intensive Treatment of Diabetes on the Development and Progression of Long-Term Complications in Insulin-Dependent Diabetes Mellitus). The DCCT study also found ongoing blood glucose control (for a period of 6.5 years) has the lasting benefit of reducing cardiovascular morbidity and mortality in people with type 1 diabetes.
Monitoring blood glucose
levels in Type 1 Diabetes Blood glucose levels can be monitored by self-monitoring or continuous glucose monitoring (CGM).
Self-monitoring of blood glucose levels
Self-monitoring is a crucial part of Type 1 Diabetes therapy. It is necessary as it can indicate the amount of insulin required for correct dosing. Self-monitoring requires the use of a glucose meter.
Continuous glucose monitoring
Most continuous glucose monitoring devices transmit blood glucose levels every five minutes. They can even alert you if you’re experiencing a hypoglycemic or hypoglycemic event. Flash glucose monitoring is one type of continuous glucose monitoring you may want to consider.
ONLY 1 IN 4 PEOPLE WITH TYPE 1 DIABETES KNOW HOW TO CONTROL THEIR NUMBERS
What are the target blood glucose levels for Type 1 Diabetes?
Below are the target blood glucose levels for Type 1 Diabetes before meals and two hours after a meal.
Target blood glucose levels for Type 1 Diabetes Mellitus.

Diet and exercise: Type 1 Diabetes
Diabetes education is essential to help Type 1 Diabetics understand how diet and exercise are crucial, and their impact on Type 1 Diabetes. Carefully planning meal and activity times is essential, as eating raises blood glucose levels while being active lowers it.
Nutrition
Carbohydrates play a crucial role in diabetes. Variations in carbohydrate intake can result in erratic blood glucose levels and hypoglycemia. When newly diagnosed with Type 1 Diabetes, it can take some time to handle carbohydrates consistency.
Some important aspects to consider when it comes to diet are:
- Estimating the amount of carbohydrate in food
- Carbohydrate counting
- Matching insulin to carbohydrate
- When to check blood glucose levels
Exercise
Regular physical activity and exercise is a significant component of diabetes management. Exercise has several benefits for all people and not just people with diabetes!
The benefits of exercise include:
- Improved blood glucose control
- Weight control
- Reduction in comorbidities hypertension, dyslipidemia, and cardiovascular disease
- Improved mood
- Improved quality of life
While exercise has not consistently been shown to improve control for patients with Type 1 Diabetes, it is important to learn how to adjust diet or insulin to accommodate exercise and avoid hypoglycemia.
Other important considerations for Type 1 Diabetes and exercise include:
- Effect of exercise on blood glucose levels
- Late hypoglycemia
- Type, intensity, and duration of exercise
- When to check blood glucose levels
- Types of snacks to have on hand to avoid hypoglycemia
What should I do next?
If you experience any symptoms of Type 1 Diabetes or risk factors for developing Type 1 Diabetes, it is important to get tested as soon as possible. We have an on-site Phlebotomist who can test you. Some people are at higher risk and need regular testing.
By diagnosing and treating Type 1 Diabetes early, it means you can decrease the risk of developing or delay any further health complications of Type 1 Diabetes, for example, nerve damage, blindness, and heart disease. It is important to know that diagnosing Type 1 Diabetes should not rely solely on using a Hb A1c test.


